Yesterday we had the pleasure of hearing 3 leaders in the world of medical simulation.
Dr. Louis Halamek, the founder and director of CAPE and a Professor of Pediatrics in the Division of Neonatal and Developmental Medicine, Department of Pediatrics, and the Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, spoke about the misinterpretation and misuse of simulation learning technology. The vast majority of universities and organizations use simulation to train young students, and don’t tap into how other industries like NASA use simulation to train and practice routine and new procedures with senior staff. CAPE is an example of a physical simulation environment where the space, equipment and even the patients (mannequins) are as close to the real thing as possible. Dr. Halamek has been involved in designing simulation mannequins and specific communication language that is used in the NICU between clinicians, and with parents when adverse outcomes happen. Dr. Halamek pointed that that what everyone wants is the delivery of safe, effective and efficient care to patients. In the US health system this is what is happening:
-Clinicians focus on their strengths.
-Clinicians take great pride in their work ethic.
-Clinicians are excellent at creating work-arounds for problems with equipment or systems.
-Clinicians often fail to address the underlying root causes of the problem…
So, what’s wrong with this? As Dr. Halamek pointed out, it’s a very reactive and superficial way to operate. Clinicians are not asking themselves (or getting support to ask themselves) “what could go wrong,” “how can it be prevented,” and “what’s the next worst thing that could happen?” Unfortunately, deviance becomes the norm.
During simulation learning, we talk about our weaknesses and how to prevent mistakes. This is the value of simulation learning. Clinicians or students are asked to complete a clinical task which is video recorded. Students/clinicians then view the simulation in a debriefing room where other experienced doctors/professors critique performance, communication and leadership skills. Too often simulation is construed as an “add-on” luxury for education both for the student and for the seasoned professional. This is the perception that Dr. Halamek is interested in changing through creating a new hospital system he calls “HOC” or Hospital Operation Center. A “Mission Control” of all hospital resources, patients and their health status. When an adverse outcome is experienced in the hospital, patient data from that incident can be uploaded to the HOC and sent to a simulation lab to run through the scenario again with the clinicians who were involved. By continuous training and honing of skills, the hospital can pin-point specific areas of care that need to be improved, thereby implementing new processes and communication protocols when needed.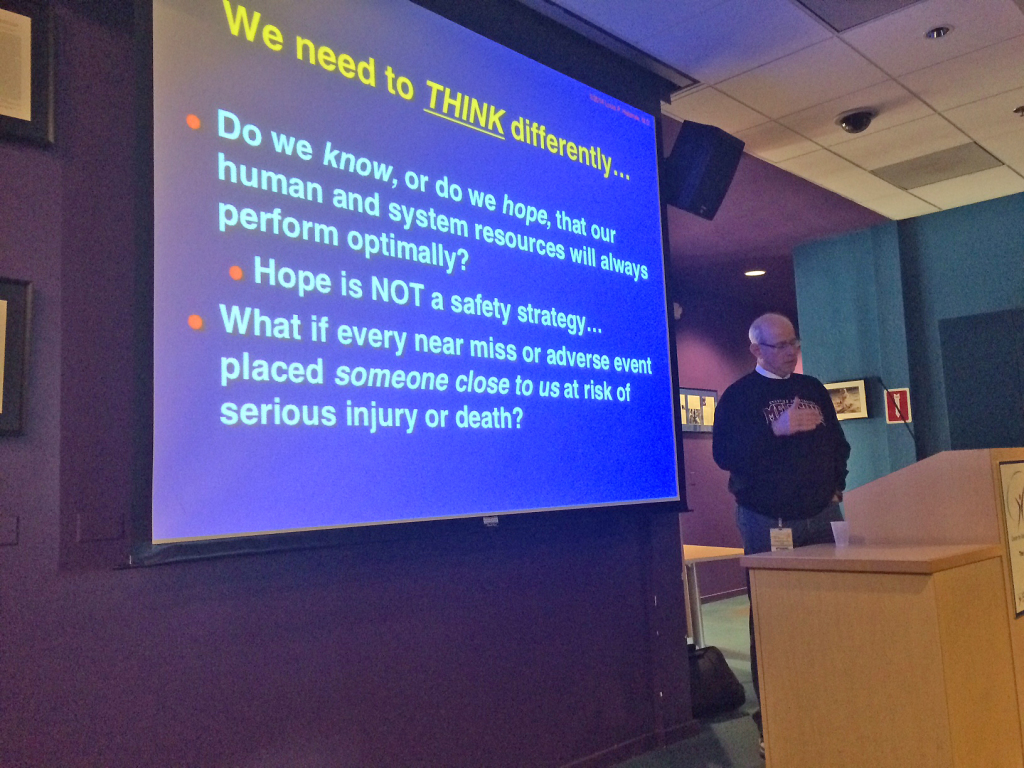 The second talk by Dr. Parvati Dev and Dr. William Heinrichs focused on virtual simulation for medical education. Both doctors have teamed up to create Clinispace. Clinispace is a virtual immersive learning environment for healthcare, disaster relief training or other kinds of training for emergency situations.
The second talk by Dr. Parvati Dev and Dr. William Heinrichs focused on virtual simulation for medical education. Both doctors have teamed up to create Clinispace. Clinispace is a virtual immersive learning environment for healthcare, disaster relief training or other kinds of training for emergency situations.

 Clinispace is inspired by multi-player video games and uses that same technology “with a medical skin.” Clinispace is ideal for learning routine clinical work or practicing system/communication protocols in dangerous work environments. This virtual mode of education is clearly very different, but as Dr. Parvati Dev noted, “Let the learning objective drive the choice of tools you use.” Very true. Thanks to all!
Clinispace is inspired by multi-player video games and uses that same technology “with a medical skin.” Clinispace is ideal for learning routine clinical work or practicing system/communication protocols in dangerous work environments. This virtual mode of education is clearly very different, but as Dr. Parvati Dev noted, “Let the learning objective drive the choice of tools you use.” Very true. Thanks to all!